Have you ever stopped to think about the intricate connections between different parts of your body? It’s truly fascinating how everything works together to keep us healthy and functioning. One such connection that often goes unnoticed is the relationship between the abducens nerve and your heart. Yes, you read that right – your eye and your heart are more connected than you might think!
Understanding the Abducens Nerve
Let’s start by unraveling the mystery surrounding the abducens nerve. This nerve, also known as cranial nerve VI, plays a crucial role in eye movement. It is responsible for controlling the lateral rectus muscle, which allows your eye to move to the side. So, whenever you look towards your temples, thank the abducens nerve for making it possible.
The abducens nerve is a fascinating component of the intricate cranial nerve system. It is one of the twelve cranial nerves that emerge directly from the brain, specifically from the pons region of the brainstem. This nerve’s unique function in controlling the lateral rectus muscle sets it apart, highlighting its importance in the realm of oculomotor control.
Anatomy of the Abducens Nerve
Before we delve deeper into the fascinating connection between the abducens nerve and your heart, let’s take a moment to understand its anatomy. The abducens nerve begins in the pons region of the brainstem and travels through the skull, eventually reaching the lateral rectus muscle of the eye. This long and winding pathway ensures that the nerve is well-positioned to carry out its important functions.
As the abducens nerve traverses through the skull, it passes through several crucial structures, including the cavernous sinus, a cavity located on each side of the sella turcica of the sphenoid bone. This intricate pathway underscores the precision and complexity of the abducens nerve’s journey from its origin in the brainstem to its target muscle in the eye.
Function of the Abducens Nerve
Now that we know where the abducens nerve is located, let’s explore its function in more detail. As mentioned earlier, this nerve allows your eye to move laterally, enabling you to gaze in different directions. It works in coordination with other cranial nerves to ensure that your eyes move smoothly and accurately, helping you to navigate the world around you with ease.
The abducens nerve’s role in facilitating horizontal eye movements is essential for activities such as reading, driving, and even simple tasks like following a moving object. This intricate coordination between the abducens nerve and other ocular muscles showcases the precision and efficiency of the human visual system.
The Connection Between the Abducens Nerve and the Heart
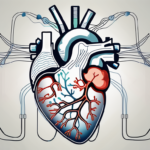
Now, here comes the surprising part – the abducens nerve’s influence doesn’t stop at your eye. It also has a subtle yet significant impact on your heart. You see, the nervous system, which includes the abducens nerve, plays a crucial role in regulating heart function.
Role of the Nervous System in Heart Function
Before we discuss how the abducens nerve specifically influences the heart, let’s take a step back and understand the broader role of the nervous system in heart function. The nervous system acts as a control center, constantly sending signals to the heart to ensure that it beats at the right rhythm and rate. It regulates everything from your heart rate to the strength of your heart muscle contractions, keeping your cardiovascular system running smoothly.
Moreover, the autonomic nervous system, a branch of the nervous system that controls involuntary bodily functions, such as heart rate, breathing, and digestion, plays a vital role in maintaining cardiovascular homeostasis. This intricate network of nerves ensures that your heart can adapt to various situations, such as exercise, stress, or rest, by adjusting its activity accordingly.
How the Abducens Nerve Influences Heart Health
Although the abducens nerve is primarily involved in eye movement, recent research has uncovered its connection to heart health. Various studies have suggested that certain disorders affecting the abducens nerve may be associated with an increased risk of heart conditions. These findings have opened up a whole new field of exploration within the fascinating realm of neurocardiology.
Furthermore, the abducens nerve’s role in heart health highlights the intricate interplay between different bodily systems. It underscores the interconnected nature of the human body, where seemingly unrelated parts can have surprising effects on one another. Understanding these connections not only sheds light on the complexity of human physiology but also paves the way for innovative approaches to diagnosing and treating various health conditions.
Potential Health Issues Related to the Abducens Nerve and Heart
Now that we know about the unexpected link between the abducens nerve and the heart, it’s essential to discuss the potential health issues that may arise in relation to these two interconnected systems.
Understanding the intricate relationship between the abducens nerve, responsible for controlling the lateral movement of the eye, and the heart, a vital organ central to our circulatory system, sheds light on the complexity of the human body’s interconnected systems. This newfound connection opens up a realm of possibilities for further research and exploration into how these seemingly distinct areas of the body may influence each other’s functioning.
Symptoms of Abducens Nerve Disorders
Disorders affecting the abducens nerve can cause a range of symptoms, including double vision, difficulty moving the eye laterally, and eye misalignment. If you experience any of these symptoms, it’s crucial to consult with a healthcare professional who can provide a proper diagnosis and guidance.
Moreover, the impact of abducens nerve disorders extends beyond ocular manifestations, potentially affecting overall neurological health and quality of life. Recognizing the early signs and symptoms of these disorders is paramount in ensuring timely intervention and management to mitigate potential complications.
Heart Conditions Linked to the Abducens Nerve
While the link between the abducens nerve and heart conditions is still being studied, initial research suggests that individuals with certain abducens nerve disorders may have an increased risk of developing heart conditions such as arrhythmias or coronary artery disease. However, it’s important to note that this connection is complex and not fully understood.
Exploring the intricate web of connections between the abducens nerve and the cardiovascular system unveils a fascinating intersection of neurology and cardiology. The potential implications of this relationship on the diagnosis and treatment of both neurological and cardiac disorders present a compelling area for future investigations and medical advancements.
Prevention and Treatment Options
Now that we’ve explored the potential health issues related to the abducens nerve and the heart, let’s discuss some prevention and treatment options that may help maintain the overall health of these interconnected systems.
Understanding the intricate connection between the abducens nerve and the heart is crucial in developing effective prevention and treatment strategies. The abducens nerve, responsible for controlling eye movement, plays a vital role in maintaining proper visual function. Meanwhile, the heart, a powerhouse organ, pumps oxygen-rich blood throughout the body, sustaining life. By prioritizing the health of these systems, individuals can enhance their overall well-being and quality of life.
Lifestyle Changes for Better Nerve and Heart Health
Adopting a healthy lifestyle can go a long way in supporting the health of both your nerves and your heart. Regular exercise not only strengthens the cardiovascular system but also promotes nerve function by enhancing blood flow and oxygen delivery. A balanced diet rich in nutrients, such as omega-3 fatty acids and antioxidants, can provide essential support for nerve health and heart function. Additionally, incorporating stress management techniques, like mindfulness meditation or yoga, can help reduce the impact of chronic stress on these delicate systems. Quality sleep is another crucial aspect of maintaining optimal nerve and heart health, as restorative sleep allows the body to repair and regenerate tissues.
Medical Interventions for Abducens Nerve and Heart Conditions
In cases where medical interventions are necessary, healthcare professionals may recommend various treatment options. These may include medications to manage symptoms, surgical interventions to correct nerve or heart issues, or other specialized procedures tailored to individual needs. Your healthcare provider will guide you through the most appropriate treatment approach for your specific condition.
It is important to seek medical advice promptly if you experience any concerning symptoms related to the abducens nerve or heart function. Early detection and intervention can significantly improve outcomes and prevent potential complications. By taking proactive steps to care for your nerve and heart health, you can safeguard these vital systems and promote a thriving, balanced lifestyle.
The Future of Neurocardiology
The exciting field of neurocardiology is continuously evolving, with new research shedding light on the intricate connections between the nervous system and the heart. Let’s take a glimpse into the future of this fascinating discipline.
Emerging Research on the Nervous System and Heart Health
Researchers around the world are working tirelessly to deepen our understanding of the connection between the nervous system and heart health. They are investigating how different nerves, including the abducens nerve, influence the heart’s functioning and the potential implications for cardiovascular health. The findings from these ongoing studies may pave the way for novel treatment approaches and preventive strategies.
One particularly intriguing area of research focuses on the role of the abducens nerve in regulating heart rate variability. Heart rate variability refers to the variation in time intervals between consecutive heartbeats, and it is an important indicator of overall cardiovascular health. Recent studies have shown that the abducens nerve, traditionally known for its role in eye movement, may also play a crucial role in modulating heart rate variability. This discovery opens up new possibilities for targeted interventions that can improve heart health and reduce the risk of cardiovascular diseases.
Innovations in Treating Nerve and Heart Disorders
Technological advancements are playing a pivotal role in treating nerve and heart disorders. From advanced imaging techniques to cutting-edge surgical procedures, these innovations are revolutionizing the way healthcare professionals diagnose and treat conditions affecting both the abducens nerve and the heart. As research continues to unfold, the future of treating nerve and heart disorders appears brighter than ever.
One promising area of innovation lies in the development of neurostimulation techniques for managing heart rhythm disorders. Neurostimulation involves the use of electrical or magnetic impulses to stimulate specific nerves, and it has shown great potential in restoring normal heart rhythm in patients with conditions such as atrial fibrillation. By precisely targeting the abducens nerve and other relevant neural pathways, neurostimulation may offer a non-invasive and highly effective alternative to traditional treatments for heart rhythm disorders.
As you can see, the abducens nerve and your heart may seem like unlikely partners, but they are indeed intricately connected. While there is still much to learn about their relationship, one thing is clear – our bodies are masterpieces of complexity and interdependence. So, the next time you marvel at the beauty of a sunset or find your heart racing with excitement, remember to thank the incredible partnership between your abducens nerve and your heart for making it all possible.